The Latest
-
Opinion
The healthcare claims system is ready for transformation. Here are 5 ways to prepare in 2026.
Artificial intelligence could rework the claims and reimbursement process, allowing faster decision-making, reduced errors and billions in savings, according to an Optum executive.
-
HCA could lose $1B from ACA subsidy lapse, Medicaid state payment decline
The for-profit hospital operator said it’s implementing a resilience plan to offset losses. Still, HCA anticipates its earnings this year will skew closely to or exceed 2025 figures.
-
Q&A
Chuck Divita on why 2026 is Teladoc’s ‘execution year’
The CEO sat down with Healthcare Dive to discuss the company’s move to accept insurance at BetterHelp, its M&A strategy and how Teladoc is using artificial intelligence.
-
Deep Dive
Health insurers brace for impact in 2026
Profits will start to tick up after reaching trough levels. Washington will play nice. M&A and AI adoption will accelerate. We asked experts to look into their crystal balls on what the coming year means for a beleaguered industry.
-
Drugs for cancer, arthritis and HIV on Medicare’s list for 2028 price cuts
Still, the medications in the latest round of negotiations — which now includes Part B drugs given in doctor’s offices — draw very limited revenue from Medicare, an analyst pointed out.
-
Elevance expects lower revenue, earnings, membership in 2026
This year should see improvements in Medicare Advantage and Affordable Care Act plans but continued pressure in Medicaid, Elevance executives warned investors.
-
CMS official defends flat Medicare Advantage rate proposal for 2027
Medicare director Chris Klomp said the Trump administration is “massively” in support of MA as health insurers cry foul over the meager rate update.
-
CMS proposes excluding chart reviews from MA risk scoring in 2027 payment rule
The proposal would eliminate the financial motivation insurers have to mine their members’ charts for additional diagnoses. Regulators also proposed a flat rate update for 2027, prompting anger from insurers.
-
Interconnectedness, extortion risk make cybersecurity a healthcare C-suite priority
A new report from Trellix reviews the biggest breaches, describes the most effective defenses and profiles the most dangerous attackers.
-
UnitedHealth revenue climbs in 2025, though profit continues to fall
The healthcare behemoth posted its lowest profits since 2018 last year, largely thanks to continued Medicare Advantage challenges. Executives warned how regulators’ “disappointing” rate update might further contract MA.
-
Surprise Billing
No Surprises disputes increasing even as arbiters catch up, CMS says
The agency released new data on independent dispute resolution in the first half of 2025. Roughly 1.2 million cases were filed in that period, mostly by the same private equity-backed providers.
-
CVS accused of shutting out rival pharmacy hubs in House Judiciary investigation
The company’s massive pharmacy benefit manager changed its rules and weaponized audits to ensure independent pharmacies couldn’t work with competing pharmacy service companies, House Republicans said.
-
31,000 Kaiser Permanente workers strike in California, Hawaii
Kaiser workers are calling for increased staffing and wages, which the union argues haven’t kept pace with rising costs. The health system said a generous offer is already on the table.
-
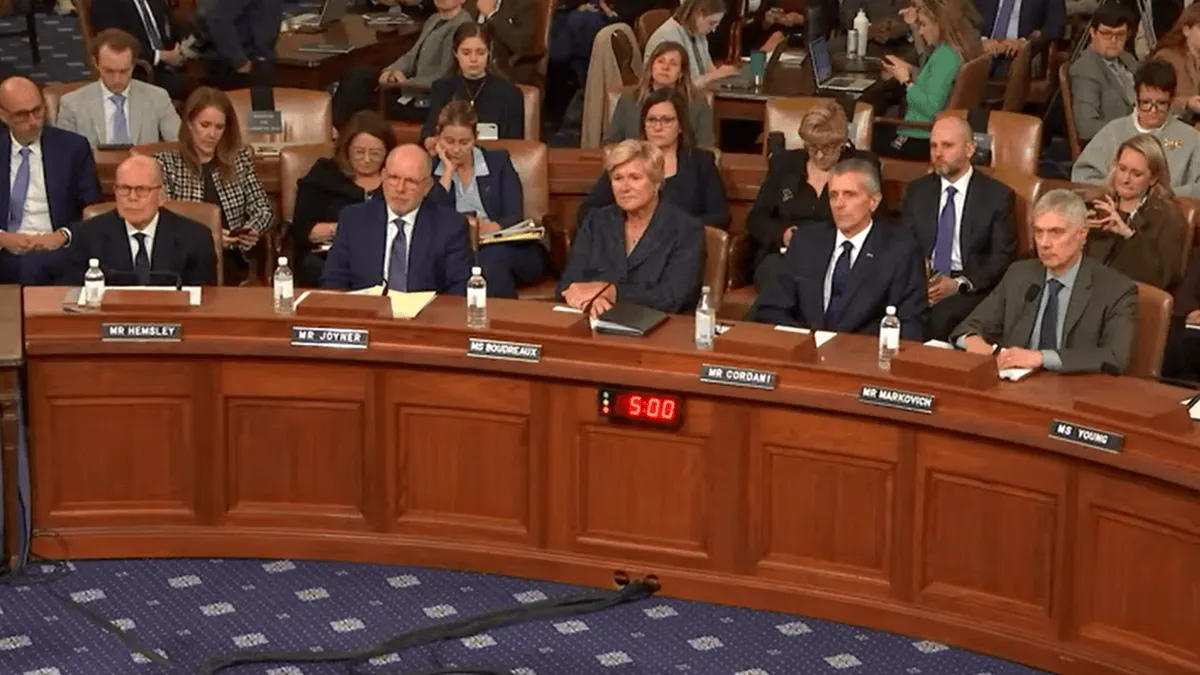
Insurance CEOs’ no good, very bad day on the Hill
The chief executives of UnitedHealth, CVS, Cigna and Elevance were pilloried for care denials, vertical consolidation and sky-high executive compensation during two House hearings Thursday.
-
Deep Dive
Top healthcare AI trends in 2026
While health systems will continue their AI rollout, use of the technology could evolve amid intensifying competition from EHRs, fragmented regulations and growing M&A opportunities.
-
Why cover GLP-1s? They’ll lower employer healthcare costs, study says
While the medications may be pricey, a multi-year study by Aon found consistent use correlates with lower medical cost growth and fewer hospitalizations for cardiovascular events.
-
Deep Dive
Top healthcare provider trends in 2026
Health systems that address costs, workforce planning and portfolio strategy may be better positioned as reimbursement headwinds intensify this year.
-
‘Shadow AI’ use is widespread in healthcare: survey
More than 40% of respondents said they were aware of colleagues using AI tools that haven’t been approved by their organizations, a potential safety and privacy risk, according to the survey by Wolters Kluwer Health.
-
Express Scripts considering settlement in FTC insulin price lawsuit
The antitrust agency paused its lawsuit against the pharmacy benefit manager while the two discuss a proposed consent agreement.
-
Congress eyes tackling healthcare consolidation
“I think there’s common ground here,” one Republican congressman said during a House Budget Committee hearing. Squaring up against healthcare monopolies would be a major pivot for the GOP.
-
Small business health insurance coverage at risk as costs rise, EBRI finds
Even as overall employer-based coverage increased in the U.S., small companies pulled back.
-
UnitedHealth pledges to return ACA profits to customers
The announcement came one day before CEO Stephen Hemsley testified on healthcare affordability in front of two congressional committees.
-
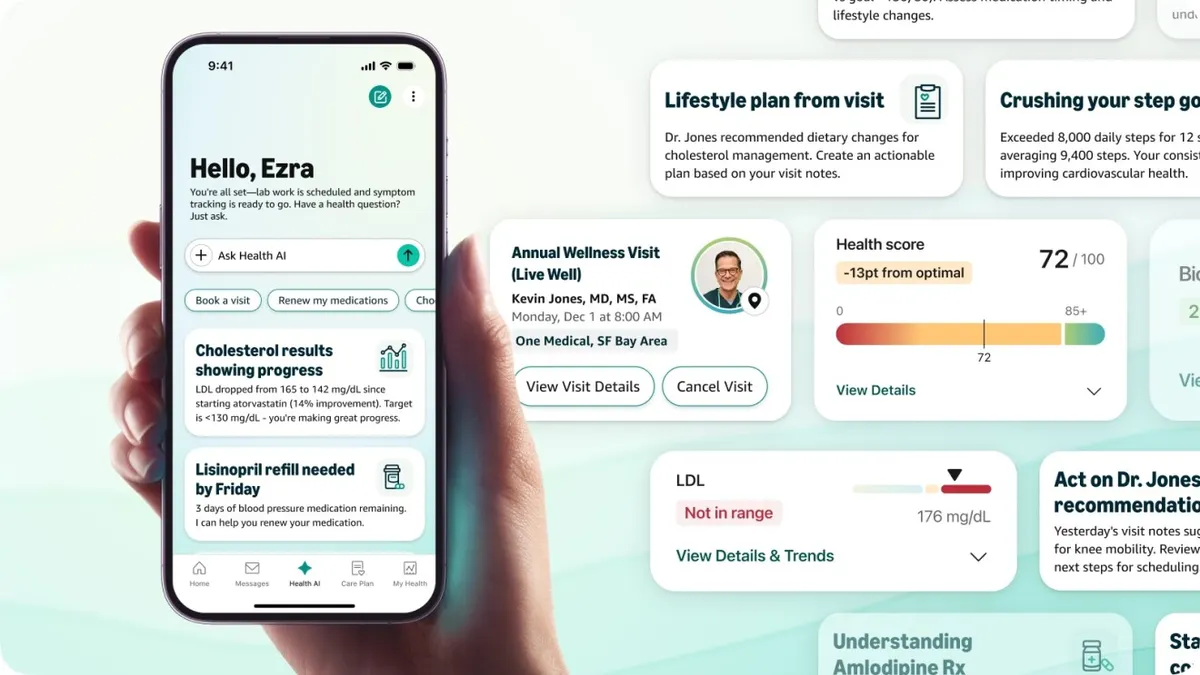
Amazon launches health AI chatbot for One Medical members
The assistant, which can answer health questions and help schedule appointments, comes on the heels of other health-focused AI tools from OpenAI and Anthropic.
-
ECRI names misuse of AI chatbots as top health tech hazard for 2026
The nonprofit said technologies like ChatGPT have suggested incorrect diagnoses, invented body parts and otherwise provided information that could lead to harm.
-
Community Health Systems to sell Alabama hospital for $450M
The for-profit hospital giant has been aggressively divesting assets as it looks to pare down debt. With the sale of Crestwood Medical Center, CHS has passed its $1 billion target for divestitures, one analyst noted.